Key Results & Achievements
WP2 and WP4 collaborated closely throughout the four-year ZikaPLAN period. Strong cross-consortium alliances were built with other researchers in South America and notably in ZIKAlliance. A large number of clinical samples including serum and viral isolates were secured for studies, and the additional funding received from MRC and Wellcome Trust was vital in contributing to this.
“Our aim is to dissect at the laboratory level to understand the molecular pathogenesis of brain infection – why this virus occurs and how it affects the survival and development of brain cells in different model systems.”
Prof. Hugh Willison, University of Glasgow
Determining ZIKV tropism and viral trafficking in murine and human PNS and CNS cultures
In terms of experimental work, Zika virus tropism in the peripheral and central nervous systems (PNS and CNS, respectively) in vitro, has been determined (Cumberworth et al 2017) and the data are informing our in vivo work (UGLAS).
The Brazilian ZIKV isolate used in this study was derived from a patient during the epidemic in Brazil in 2015. We found that oligodendrocytes and oligodendrocyte precursors cells were most susceptible to infection after 24h. These cells are the myelinating cells of the CNS and provide nerve fibres with insulation for an efficient neuronal conduction. When infecting cultures during the process of myelination, we observed cell death and the pathology of white matter structures. This has major implications for the health of the developing brain. In particular, the demonstration that oligodendrocytes can be infected has implications for the possible effects of childhood infection on the postnatal developing brain.
Further investigations showed that ZIKV also affects CNS cells after myelination and causes demyelination and axonal pathology (UGLAS, Schultz et al submitted). Time-course studies revealed that myelin damage occurs as early as glial cells, such as oligodendrocytes, are infected. We employed transcriptomic analysis (RNA sequencing) to determine factors involved and found, in addition to an antiviral response, molecules known for processes of neuroinflammation and demyelination. Supernatant transfer experiments showed that the pathology is a direct effect of active viral replication (UGLAS, Kohl group (ZIKAlliance) Schultz et al. submitted). This work has implications for the understanding of ZIKV infections in the post developmental CNS, for which neuropatholgies such as myelitis, encephalitis, meningoencephalitis and encephalomyelitis have been reported.
In vitro studies undertaken in Glasgow showed that infection of CNS cells leads to a secondary axonal phenotype, in the absence of productive infection of neurons. A common molecule involved in the final step in axonal death is SARM1 (Sterile alpha and TIR domain containing protein), which is being examined as potential link between viral infection of neighbouring glial cells and axonal pathology. Our current data show that ZIKV-mediated axonal death involves SARM1. We currently aim to determine if this is due to accumulation of substrate or depletion of the enzyme’s product, NAD+. This work reveals a target molecule involved in ZIKV induced CNS injury and impacts the development of anti-viral therapies.
KUL established an in vitro model of ZIKV infection in different types of human induced pluripotent stem cell (iPSC)-derived neural cells: cortical neurons, motor neurons and astrocytes. Strains from both the African and the Asian lineage are able to productively infect these stem cell-derived neural cells and cause cytopathic effects, result in production of infectious viral particles and lead ultimately to cell death. Interestingly, ZIKV infection in these neuronal cells was efficiently inhibited by the direct-acting antiviral compound 7-deaza-2′-C-methyladenosine (7DMA), but not by favipiravir (T-705) or ribavirin. The inhibition resulted in reduced viral loads and longer survival of the cells. Infection of induced pluripotent neural stem cells can be used to successfully perform drug screens and assist in finding treatments for ZIKV infection of the nervous system.
Determining the pathological consequences of ZIKV infection in the nervous system in vivo
Based on our observations in vitro, we infected mice during developmental myelination (UGLAS). This is a time when neurogenesis is largely complete and neurons are less susceptible to infection by ZIKV. Systemic infection of postnatal day (P) 5-6 mouse pups (CNS myelination begins at P1 and is largely complete by P60 in mice; 3rd trimester to 2 years of age in humans) with ZIKV led to the infection of CNS glial cells (Schultz et al., submitted). A similar infection pattern and vulnerability of cells was observed, when comparing our in vivo data to our in vitro studies. These data have implications for understanding neurodevelopmental delays in congenitally infected infants who appeared asymptomatic at birth.
Different viral isolates showed different tropism for nervous system cells in vitro (UGLAS and Kohl group (ZIKAlliance)) and in vivo (Schultz et al., submitted). KU Leuven together with Institute Pasteur compared the pathogenicity of a selection of low-passage ZIKV strains from both the Asian and African lineage, which represent the recently circulating viral genetic diversity, in adult mice (Aubry et al., submitted; preprint available at BioRxiv). The African ZIKV strains were significantly more lethal than their Asian counterparts ZIKV strains, i.e. mice infected with African ZIKV succumbed significantly earlier than those infected with Asian ZIKV. Viral RNA levels in organs (including brain and spinal cord) collected on day 7 post infection were also consistently higher for mice infected with the African ZIKV strains. In collaboration with the University of Liège (ZIKAlliance), a recent model of ZIKV-induced microcephaly by intraplacental injection in mouse embryos was employed to investigate the vertical transmission phenotypes for one ZIKV strain from the African lineage and two ZIKV strains from the Asian lineage. The African strain caused massive resorption resulting in the death of all infected embryos harvested at E18.5. In contrast, both Asian strains resulted in pronounced microcephaly and ventriculomegaly at E18.5. Of note, a difference in severity was also observed between the two Asian ZIKV strains. Altogether, these data demonstrate the high pathogenicity of the recent ZIKV strains from Africa. These findings contribute to the understanding of ZIKV evolution.
Identifying and characterizing ZIKV receptors on human neural cells to explain ZIKV neural tropism and pathogenesis
Good progress was made in characterizing the nature of Zika virus’ main cellular receptors on human neural cells, with suspected and unknown candidates being investigated (UmU). To identify host factors of importance for ZIKV infection, we have used the 60 cell lines developed by the US National Cancer Institute, “NCI-60”, which have been mapped/characterized by micro array for mRNA expression. We infected these cells, with ZIKV, and compared ZIKV cell killing capacity. This provided a “foot print”, which have been analyzed against the mRNA expression database provided online by US NCI. With the NCI-60 screen being the first screen aiming to identify genes important for infection and not only transduction we decided to compare our list of genes with two already published screens, one full genome CRISPR/Cas9 based screen as well as a pulldown/masspec based screen. When combining the data of these three screens we found three overlapping genes that are present in all screens, namely CS, KTN1 and BAF45b. The knockout of KTN1 and BAF45b in vitro reduced the transduction of ZIKV by 60% and 95%, respectively. Early mechanistic studies have indicated that BAF45b KO is not reducing viral attachment/entry but rather prevents the replication of viral RNA as no dsRNA intermediate is produced. Further, strand specific RNA analysis using qPCR revealed that the production of negative sense RNA is severely impaired. BAF45b encodes a protein that is a part of the BAF complex that is crucial for regulation of gene expression and differentiation. In addition, the BAF complex is important for a normal differentiation of a neuronal stem cell into a neuron. This work has implications for the understanding of mechanisms related to viral replication and host factors used by ZIKV for infection of human target cells. Additionally, this knowledge contributes to novel drug development.
Studies to investigate whether humoral factors from Zika-GBS patient and control sera are pathogenic to PNS and CNS cells in vitro also progressed well (UOXF). Zika GBS samples are showing evidence of co-associating with anti-neural antibodies in PNS targeted assays. These studies are being followed up with target identification and validation studies where sufficient sample volumes are present.
Sera from Zika-GBS cases and controls were screened for antigen targets known to be associated with conventional GBS using sensitive immunoassays (UGLAS): to date these have not been found, indicating the Zika-GBS may have a unique autoimmune signature. Investigations are therefore continuing using different in vitro culture systems.
Comparing immune responses in non-neurological ZIKV infection, viral invasion of the CNS (e.g. encephalitis) and auto-immune neurological disease
The aim of this task is to characterize the host immune response in Zika-associated neurological disease (ULIV and Fiocruz). The cellular studies to examine differential immune responses in patients with non-neurological ZIKV infection, patients with viral invasion of the CNS (e.g. encephalitis) and patients with autoimmune neurological disease began once the collection of carefully archived clinical samples launched by WP2 was completed. Serum and whole blood samples are being stored systematically in biobanks in Brazil for subsequent characterisation of cytokine, chemokine and metabolic biomarkers of GBS and encephalitis; transcriptional inflammatory signatures and other immunological characterisation of patient cell populations. From patients in these cohorts peripheral blood mononuclear cell (PBMC) samples were collected. In collaboration with partner LJI, several T cell epitopes of Zika have been mapped (Grifoni et al, JVI 2017). Understanding the cellular and humoral immunology of Zika infection has potential implications for vaccine design and biomarker discovery.
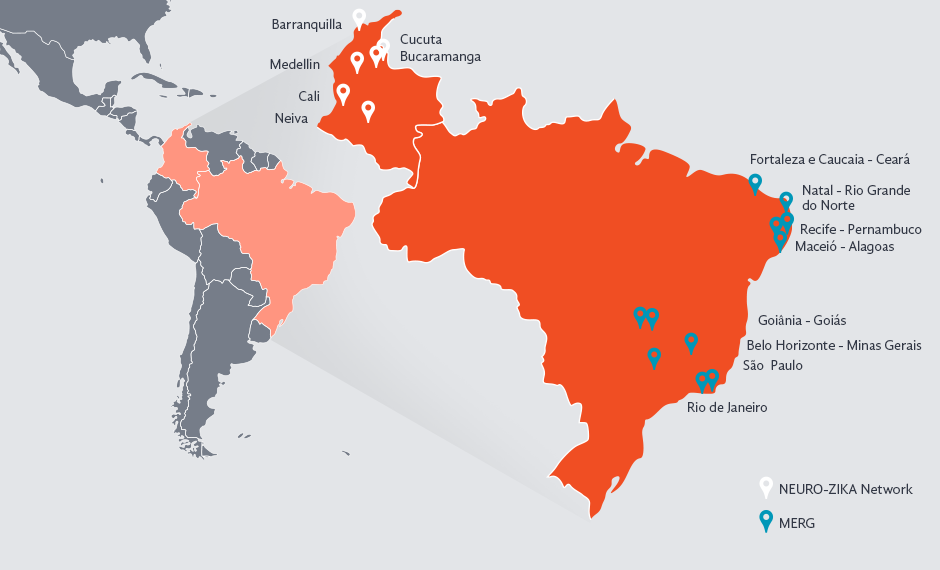
MERG and NEURO-ZIKA Networks
Participating Organisations
Group leader: Prof. Hugh Willison, University of Glasgow
- Umeå University
- University of Leuven (KU Leuven)
- The University of Liverpool
- La Jolla Institute for Allergy and Immunology
- Fundação Oswaldo Cruz (Fiocruz)